This year’s AML (acute myeloid leukemia) World Awareness Day on April 21, 2019, marks the continued evolution of promising treatment possibilities for patients with AML. Recent biomarker identification and targeted therapy approvals have inaugurated a new outlook for patients with AML under the auspices of precision medicine. Previously beset with poor overall survival rates, AML is now treated with targeted therapies that are extending lives. But the success of these treatments depends entirely on vigilant and timely testing with the right test at the right time. It also means testing again if relapse occurs.
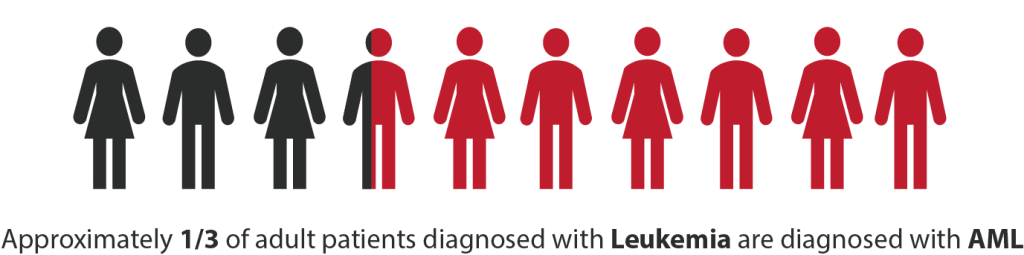
AML, which affects approximately 30% of patients with leukemia,1 is a rapidly developing cancer that requires immediate and appropriate treatment. Misdiagnoses and delayed treatment can mean the difference between life and death for patients, for whom the 5-year overall survival rate is only 25%.1 This is why getting the right test at the outset, and again if relapse occurs, is so critical. 
New treatments for AML target genetic abnormalities in blood cells that characterize AML. Some of the genes that are commonly identified as abnormal in AML include FLT3, IDH1, and IDH2.2-4 For example, approximately one-third of patients with AML have FLT3-internal tandem duplication (ITD) mutations, which indicate a particularly poor prognosis for patients.5-9 By identifying biomarkers and genetic mutations such as FLT3 through genetic* testing, physicians are now able to tailor treatment plans to patients with AML with targeted therapies that target these individual genetic abnormalities on a patient-by-patient basis. For example, targeted therapy for patients with FLT3 mutations is initiated with chemotherapy. Similarly, separate targeted therapies are indicated for patients with the IDH1 or IDH2 gene mutations who did not respond to initial therapy (refractory) or who relapsed after initial therapy.
Since targeted therapy is effective only when given to patients identified as having the certain biomarker the treatment targets, it is imperative that genetic testing occur at diagnosis. But testing only at diagnosis is not enough. Mutational status can change within individual patients. Specifically, because of clonal evolution in AML, mutational status may change in patients after relapse.10-13 For example, FLT3 is not a stable biomarker and may not show up at diagnosis.14 However, it can emerge after relapse, making it imperative that patients be tested for the presence of FLT3 mutations not just at diagnosis but also at relapse.14 This means new treatment options may be considered after diagnosis if patients relapse, which is a crucial development as many patients with AML die from progressive disease following relapse.15 If new mutations are identified after relapse, new targeted treatments can be applied to improve health outcomes. But those mutations won’t be identified without vigilant testing.
*Also referred to as molecular testing.
References
- Howlader N, Noone AM, Krapcho M, et al. SEER Cancer Statistics Review, 1975–2014, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2014/, based on November 2016 SEER data submission, posted to the SEER web site, April 2017.
- Döhner H, Weisdorf DJ, Bloomfield CD. Acute myeloid leukemia. N Engl J Med. 2015;373(12):1136-1152.
- Papaemmanuil E, Gerstung M, Bullinger L, et al. Genomic classification and prognosis in acute myeloid leukemia. N Engl J Med. 2016:374(23):2209-2221.
- Kumar CC. Genetic abnormalities and challenges in the treatment of acute myeloid leukemia. Genes Cancer. 2011 Feb;2(2):95-107.
- Fröhling S, Schlenk RF, Breitruck J, et al. Prognostic significance of activating FLT3 mutations in younger adults (16 to 60 years) with acute myeloid leukemia and normal cytogenetics: a study of the AML Study Group Ulm. Blood. 2002;100(13):4372-4380.
- Patel JP, Gönen M, Figueroa ME, et al. Prognostic relevance of integrated genetic profiling in acute myeloid leukemia. N Engl J Med. 2012;366(12):1079-1089.
- Schlenk RF, Döhner K, Krauter J, et al. Mutations and treatment outcome in cytogenetically normal acute myeloid leukemia. N Engl J Med. 2008;358(18):1909-1918.
- Schlenk RF, Kayser S, Bullinger L, et al. Differential impact of allelic ratio and insertion site in FLT3-ITD-positive AML with respect to allogeneic transplantation. Blood. 2014;124(23):3441-3449.
- Fathi AT, Chen Y-B. Treatment of FLT3-ITD acute myeloid leukemia. Am J Blood Res. 2011; 1(2): 175–189.
- Warren M, Luthra R, Yin CC, et al. Clinical impact of change of FLT3 mutation status in acute myeloid leukemia patients. Mod Pathol. 2012;25(10):1405-1412.
- Kottaridis PD, Gale RE, Langabeer SE, Frew ME, Bowen DT, Linch DC. Studies of FLT3 mutations in paired presentation and relapse samples from patients with acute myeloid leukemia: implications for the role of FLT3 mutations in leukemogenesis, minimal residual disease detection, and possible therapy with FLT3 inhibitors. Blood. 2002;100(7):2393-2398.
- Shih L-Y, Huang C-F, Wu J-H, et al. Internal tandem duplication of FLT3 in relapsed acute myeloid leukemia: a comparative analysis of bone marrow samples from 108 adult patients at diagnosis and relapse. Blood. 2002;100(7):2387-2392.
- Cloos J, Goemans BF, Hess CJ, et al. Stability and prognostic influence of FLT3 mutations in paired initial and relapsed AML samples. Leukemia. 2006;20(7):1217-1220.
- Daver N, Schlenk RF, Russell NH, Levis MJ. Targeting FLT3 mutations in AML: review of current knowledge and evidence. Leukemia. 2019 Feb;33(2):299-312.
- Ding L, Ley TJ, Larso DE, et al. Clonal evolution in relapsed acute myeloid leukemia revealed by whole genome sequencing. Nature. 2012 Jan 26; 481(7382): 506–510.
